Tummy Bug Science
Below we will discuss the science behind the content in Matty Macrophage & the Tummy Bug!
(Disclaimer: This does not constitute medical advice. Please consult your physician for information regarding your medical care.)
Macrophage
type of white blood cell (WBC) that detects, phagocytoses (eats), and destroys substances foreign to the body as well as presents antigens (substances that induce an immune response/body’s protective reaction to foreign invaders) to other cells ; originates from monocytes (another type of cell in the body) and leaves the circulation to differentiate/change into more specialized “fighter” cells
Neutrophil
type of WBC that acts as a “first responder” to foreign invaders in the body, particularly bacteria and cancer cells; destroys these foreign invaders via phagocytosis (eating)
Eosinophil
type of WBC that fights parasites as well as being associated with allergy and asthma; on microscopic examination they have a bilobed (two lobes) nucleus and (after staining with a chemical called eosin) red granules (Izzie’s two eyes and freckles!)
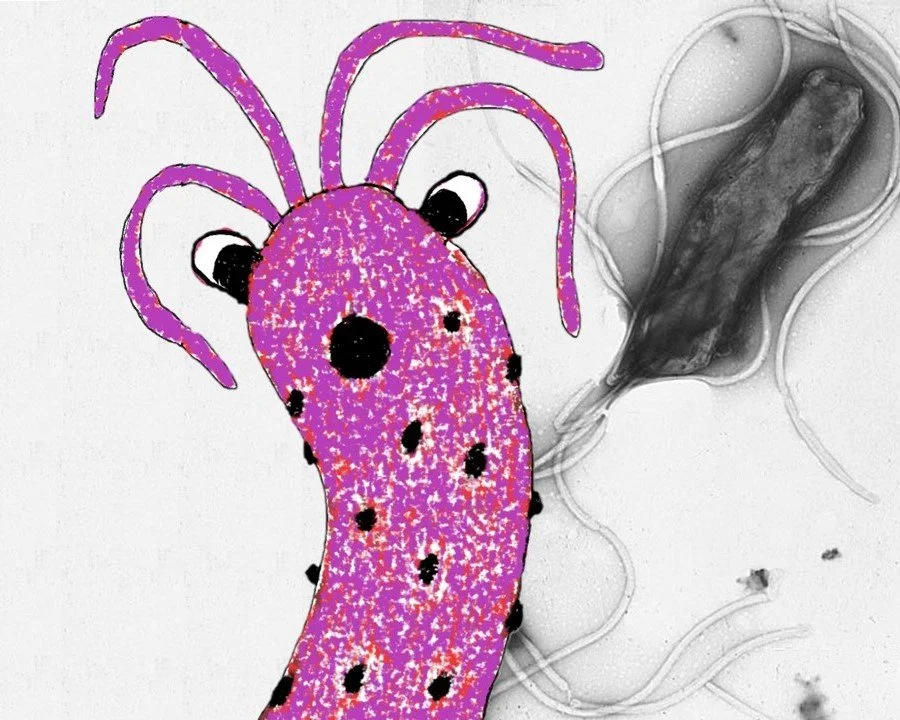
Helicobacter pylori (H. pylori)
type of bacteria (Gram negative) that although often asymptomatic, can cause gastritis (inflammation of the stomach), stomach & duodenal ulcers, & cancer
Red blood cell (RBC)
type of cell that carries oxygen from the lungs to the body’s tissues via the circulatory system (collection of blood vessels)
Parietal cell
type of cell located in the stomach that secretes hydrochloric acid and intrinsic factor
Osteoblast
type of cell that forms bone tissue, synthesizing and secreting bone matrix and participating in bone mineralization
Bone marrow
type of tissue found in the center of most bones; composed of red & yellow marrow types; red marrow contains stem cells that can develop into RBCs, WBCs, or platelets (cells that form clots to help stop bleeding); yellow marrow contains fat as well as stem cells that can develop into cartilage, fat, or bone cells; marrow is basically the place where many cells are “born”
Blood vessel
tube or channel through which the blood of the body circulates
Blood
fluid found in the body that delivers oxygen and nutrients to the tissues and removes wastes; composed of plasma and blood cells
Stomach
an organ found between the esophagus and small intestine that is responsible for the chemical breakdown of food by means of enzymes and hydrochloric acid
Pathophysiology of H. pylori infection:
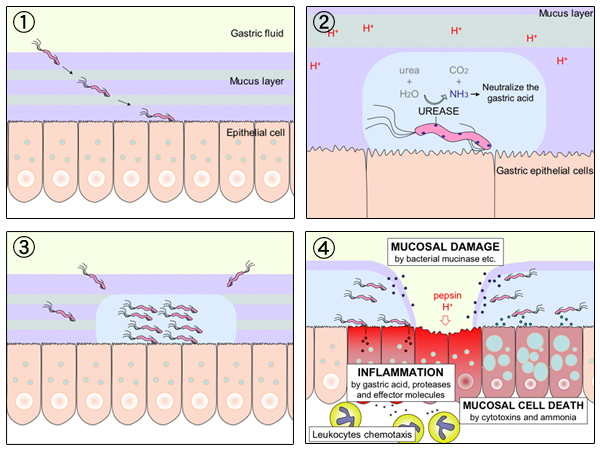
Helicobacter pylori is a Gram negative, microaerophilic (requires environments with lower amount of oxygen than in the Earth’s atmosphere) bacterium usually found in the stomach. It has a helical (spiral) shape that is thought to help it invade the mucoid lining of the stomach. This bacterium uses its flagella to burrow into the mucus lining of the stomach to reach the less acidic epithelial cells underneath, where it will reside either in the overlying mucus, inner surface of the epithelium, or in the epithelial cells themselves. The bacterium also protects itself by neutralizing the acid in the stomach by secreting an enzyme called urease. The bacterium can then harm the stomach (as well as a part of the small intestine called the duodenum) by damaging the epithelial cells, leading to inflammation (gastritis in the stomach) and ulcers. Inflammation caused by H. pylori is thought to be a cause of carinogenesis (cancer formation). H. pylori is infectious and is thought to be transferred by either the oral-oral (kissing, mouth feeding, etc) or fecal-oral (not washing hands after the restroom, unclean water supply, etc) routes.
Complications from H. pylori infection:
H. pylori is usually asymptomatic (no symptoms), but can cause gastritis or duodenitis (inflammation of the stomach and duodenum, respectively). Approximately 10-20% of people with H. pylori will ultimately develop gastric and duodenal ulcers. H. pylori has been associated with cancer of the mucosa-associated lymphoid tissues (MALT) in the stomach, esophagus, colon, rectum as well as tissues around the eye (extranodal marginal zone B-cell lyphoma), and of lymphoid tissue in the stomach (diffuse large B-cell lymphoma). H. pylori is associated with a 1-2% lifetime risk of stomach cancer and less than a 1% risk of gastric MALT lymphoma.
Diagnosis of H. pylori:
There are noninvasive and invasive tests for the bacterium. Noninvasive tests include: blood antibody tests, stool antigen tests, and the carbon urea breath test. The invasive test is a endoscopic biopsy combined with either a rapid urease test or microbial culture.
Treatment of H. pylori infection:
The body tries to prevent colonization of H. pylori in the stomach; however, once colonization has occurred various regimens are necessary for effective treatment. The first line treatment is considered to be a triple-drug therapy consisting of the antibiotics clarithromycin and amoxicillin as well as a proton-pump inhibitor (like omeprazole) that is given for 14-21 days.
Q&A Section:
Question: How did Matty & friends get rid of the Bug? Don’t you need antibiotics for a bacterial infection?
Answer: Matty & friends were able to get the Bug (H. pylori) out of the stomach before adherence and colonization. From Testerman et al: “Transmission of H. pylori, however, appears to be infrequent, requiring the organism to take hold quickly and avoid being swept into the intestine. This makes adherence a critical early step in colonization. Colonization can therefore be viewed as the confluence of mechanisms used to persist in the stomach.” If adherence and colonization occurred leading to pathologic sequelae, pharmacotherapeutics would need to be employed, which would include an antibiotic regimen.
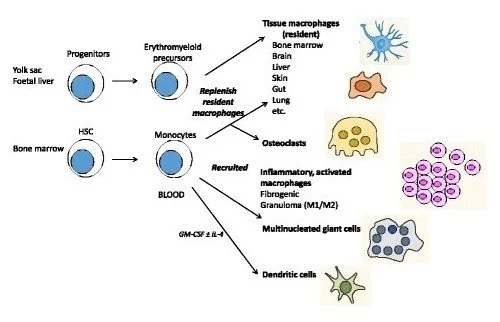
Question: What is the relationship between monocytes and macrophages?
Answer: Monocytes are a type of WBC produced in the bone marrow that subsequently circulate in the bloodstream and can migrate into tissues and differentiate into macrophages or dendritic cells. Monocytes themselves also can undergo phagocytosis, antigen presentation, or cytokine production. Macrophages are a type of WBC that are either derived from circulating monocytes or are established before birth and maintained independently of monocytes.
Question: Are there macrophages in the bone marrow? Should Matty be a macrophage or a monocyte?
Answer: Yes, there are macrophages in the bone marrow. These macrophages help control and/or promote the homeostasis in bone and bone marrow as well as other functions such as hematopoiesis (RBC formation). Concerning Matty, most of the macrophages that accumulate at diseased sites typically are derived from circulating monocytes as these monocytes undergo leukocyte extravasation, a process by which the monocytes enter damaged tissues through the endothelium of blood vessels. However, there is another group of macrophages found in the bone marrow (and other locations in the body) that are derived from embryonic yolk sac and fetal liver precursors. In the story/series, Matty is “at home” in the bone marrow whereupon he meets Jimmy, a neutrophil. At that point, Matty could either be a tissue macrophage from a embryonic precursor or a monocyte that has yet to travel to the site of pathology and differentiate into a macrophage. For literary purposes and the sake of simplicity, we have identified Matty as a macrophage that will respond to pathologies throughout the body while still calling “The Marrow” (or bone marrow) his home, acknowledging that the human body is much more complex than what is depicted via science fiction.
From Gordon et al. Tissue macrophages: heterogeneity and functions. BMC Biology. 15, Article number: 53 (2017).
Question: Do eosinophils respond to H. pylori infections? Aren’t they just involved in parasitic infections, allergic reactions, or cancer?
Answer: Although most commonly associated with parasites, allergies, and cancer, it has been shown that eosinophils increase in the stomach in H. pylori infection; therefore, making Izzie’s presence in the stomach during an H. pylori infection appropriate physiologically.
Question: Why does Jimmy have a headband?
Answer: He is a (head)band neutrophil! A band neutrophil is an immature neutrophil with a curved and not lobular nucleus. Usually there is an increase in the number of these immature neutrophils (called bandemia and representing a “left shift”) in infectious or inflammatory conditions.
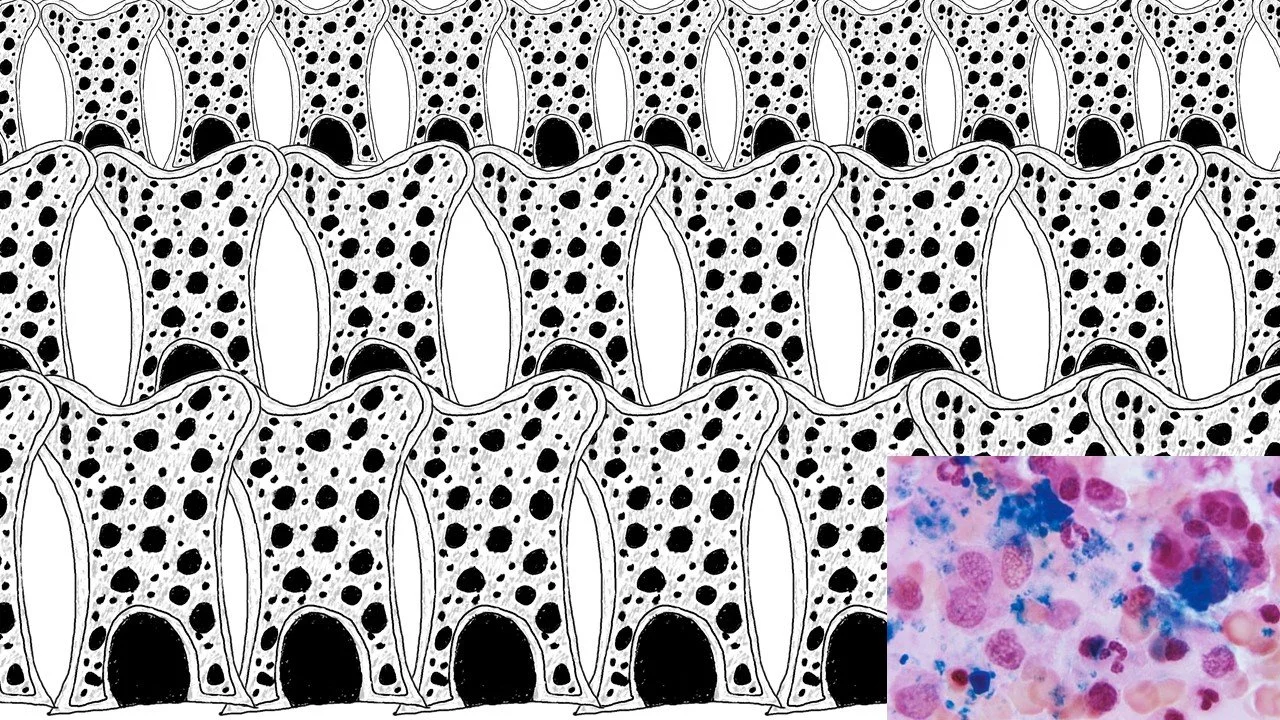
Neutrophil band cell
Notice how the nucleus (darker material) is curved rather than lobular.
Question: Why does the story say “opened his eyes” and “eyes did water”? I thought Matty had only one eye corresponding to his one nucleus. Is the plural “eyes” wrong?
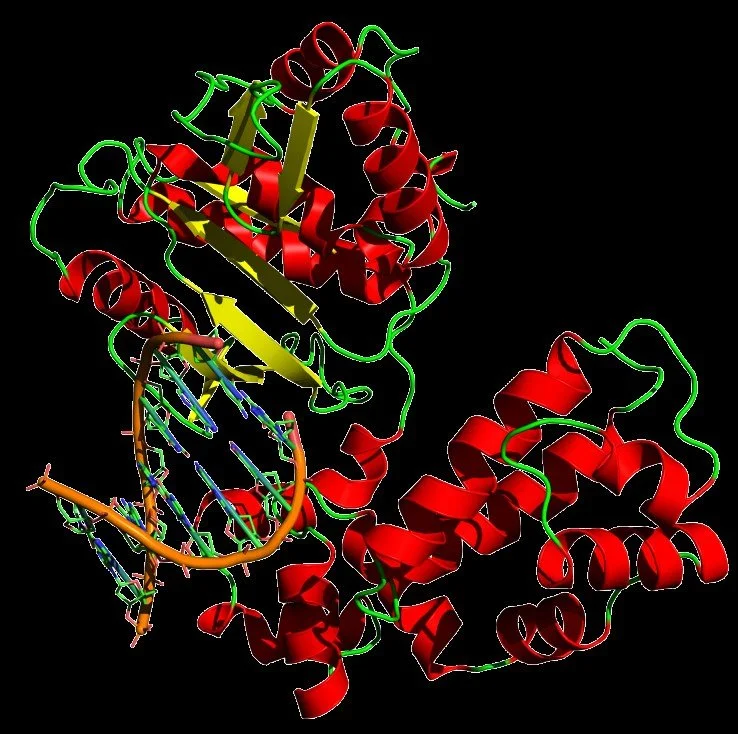
Answer: You are correct! It is wrong and we made a mistake! Thinking of basic human anatomy while writing the story, “eyes” was written in the plural form rather than the singular form “eye” as it should have been. You have found our mistake! We can also see in biology “mistakes” made with mutations - something we might see in a later book - happening during DNA replication or caused by environmental factors. These are often found and corrected during DNA replication by the proofreading exonuclease activity of DNA polymerase but some can sneak by! The important thing with mistakes is how you acknowledge and learn from them. We humbly acknowledge our conceptual error and will strive to do better!
DNA polymerase
This enzyme catalyzes the synthesis of DNA molecules from nuceloside triphosphates (i.e., adenine, guanine, cytosine, & thymine) by forming base pairs. The process is not quite perfect, as the enzyme makes one mistake for every billion base pairs copied. When an incorrect pair is recognized the enzyme moves backwards, excises the incorrect pair with exonuclease activity (a process known as “proofreading”), and then re-inserts the correct base pair and replication continues. In our story, we added an extra “s” twice, which would of happened in the human body after 1 quintillion of base pairs were copied! We have a lot more words to write to catch up to the human body!
Question: Does H. pylori increase or decrease gastric acid?
Answer: As with many things in science & pathophysiology, it depends: “Helicobacter pylori infection increases gastric acid secretion in patients with duodenal ulcers but diminishes acid output in patients with gastric cancer and their relatives.” There are specific cytokines released during H. pylori gastritis (inflammation of the stomach) that result in an increase in acid secretion; however, the ability to secrete acid depends on the state of the gastric mucosa: “The net effect of corpus gastritis is to decrease acid secretion” & “Specific products of H. pylori inhibit parietal cells.” Another interesting fact is that the location of H. pylori colonization in the stomach depends on the acidity of the stomach. “In people producing large amounts of acid, H. pylori colonizes near the pylori antrum (exit to the duodenum)” - like in our story! - “to avoid the acid-secreting parietal cells of the fundus (near the entrance to the stomach).” “In people producing normal or reduced amounts of acid, H. pylori can also colonize the rest of the stomach. The inflammatory response caused by bacteria colonizing near the pylori antrum induces G cells in the antrum to secrete the hormone gastrin, which travels through the bloodstream to parietal cells in the fundus. Gastrin stimulates the parietal cells to secrete more acid into the stomach lumen, and over time increases the number of parietal cells, as well. The increased acid load damages the duodenum, which may eventually result in ulcers forming in the duodenum. When H. pylori colonizes other areas of the stomach, the inflammatory response can result in atrophy of the stomach lining and eventually ulcers in the stomach. This may also increase the risk of stomach cancer.” So, in short, H. pylori can do both!
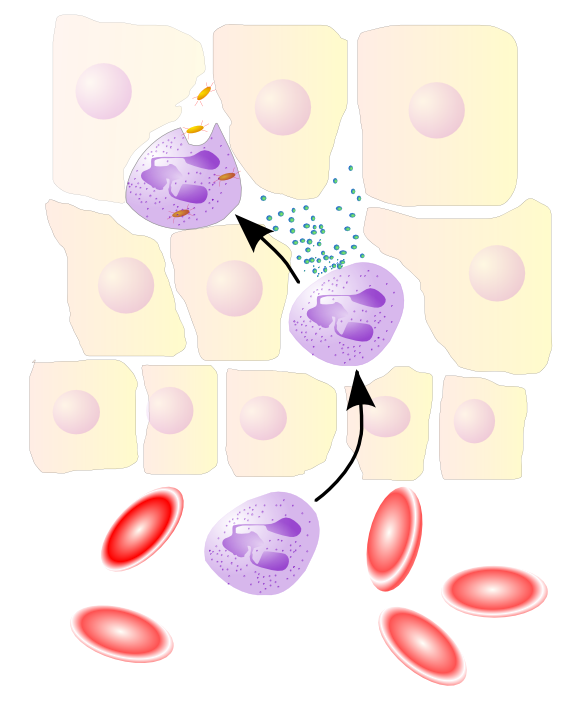
Question: How would Matty & his friends arrive to the stomach? Does the blood vessel rapids turn into the acid churning waves? Do they ride in a boat?
Answer:
The above diagram is very complex, but we will try to simplify it! Cells of the stomach recognize the H. pylori bacterial infection. They secrete chemicals that attract the inflammatory cells (i.e., neutrophils, macrophages, etc) to travel to the site of infection via blood vessels (process called leukocyte chemotaxis). Once at the site of infection, the inflammatory cells have to leave the blood vessels to enter the damage tissue. They do this by a process known as leukocyte extravasation (aka leukocyte adhesion cascade or diapedesis).
leukocyte extravasation, aka leukocyte adhesion cascade or diapedesis
Although theatrically fun for storytelling processes, the immunological cells do not have a boat to sail! (The boat sailing actually represents the process of leukocyte chemotaxis as mentioned above.)
Synopsis of H. pylori infection and the body’s immune response!
References:
By Mikael Häggström, MD. Signet-ring-cell-like foamy macrophage and normal macrophage. Wright stain. Sample from cerebrospinal fluid. 28 August 2022. Public Domain (CC0 1.0).
By User CS99 at German Wikipedia. Neutrophile segmented Granulocyte. 1 October 2005. Public Domain.
By User CS99 at German Wikipedia. Eosinophile Granulocyte. 1 October 2005. Public Domain.
By Zvesoulis. Electron micrograph of H. pylori possessing multiple flagella (negative staining). Photo from http://info.fujita-hu.ac.jp/~tsutsumi/photo/photo002-6.htm Contributed with full permission from: Yutaka Tsutsumi, M.D. Professor Department of Pathology Fujita.
By E rulez. This image was copied from wikipedia:nl. The original description was: rode en witte bloedcel - http://web.ncifcrf.gov/ - PD {| border="1" ! date/time || username || edit summary |---- | 21 sep 2004 10:38 || Svdmolen || <nowiki>(rode en witte bloedcel -. 9 November 2005. Public Domain.
By Mikael Häggström, MD. A parietal cell. 7 August 2020. From the (medical) gallery of Mikael Häggström, MD. Last updated: 2022-10-11. Licensing (unless other license is given for image): Creative Commons CC0 1.0 Universal Public Domain Dedication, used with permission.
By Nephron. Very high magnification of “bone in hypercalcemia.’ H&E stain. Brown tumour is present. Brown tumours are lesions that result from hypercalcemia. They are not true neoplasms. (Meydan N, Barutca S, Guney E, et al. (June 2006). “Brown tumors mimicking bone metastases”. J Natl Med Assoc 98 (6): 950–3. PMID 16775919. PMC: 2569361.) 23 May 2012. Creative Commons Attribution-Share Alike 3.0 Unported license.
By Dr. Gordon D. McLaren. This photograph of a Prussian blue stained bone marrow sample, revealed that there was a normal amount of iron stores. Normal iron stores are seen as dark blue-stained material in the bone marrow. 1972. https://phil.cdc.gov/details_linked.aspx?pid=2657. Uploaded by Kuon.Haku. 21 January 2021. Public Domain.
By Lord of Konrad. Cross of a human artery. 10 December 2009. Public Domain.
By FastilyClone. Author’s own picture. Digital camera shot of human (pyloric)stomach through a microscope. 13 July 2016. Public Domain.
Helicobacter pylori. Wikipedia. https://en.wikipedia.org/wiki/Helicobacter_pylori. Accessed 7 November 2022.
Testerman TL, McGee DJ, Mobley HLT. Adherence and Colonization. In: Mobley HLT, Mendz GL, Hazell SL, editors. Helicobacter pylori: Physiology and Genetics. Washington (DC): ASM Press; 2001. Chapter 34.
Monocyte. Wikipedia. https://en.wikipedia.org/wiki/Monocyte. Accessed 7 November 2022.
Macrophage. Wikipedia. https://en.wikipedia.org/wiki/Macrophage. Accessed 7 November 2022.
Kaur et al. Role of bone marrow macrophages in controlling hemostasis and repair in bone and bone marrow niches. Semin Cell Dev Biol. 2017 Jan;61:12-21. doi: 10.1016/j.semcdb.2016.08.009. Epub 2016 Aug 10. PMID: 27521519.
de Back et al. Of macrophages and red blood cells; a complex love story. Front. Physiol. 30 January 2014. Sec. Membrane Physiology and Membrane Biophysics. https://doi.org/10.3389/fphys.2014.00009.
Gordon et al. Tissue macrophages: heterogeneity and functions. BMC Biology. 15, Article number: 53 (2017).
Aydemir et al. Eosinophilic infiltration, gastric juice and serum eosinophil cationic protein levels in Helicobacter pylori-associated chronic gastritis and gastric ulcer. Mediators Inflamm. 2004 Dec; 13(5-6): 369-372. doi: 10.1155/S0962935104000559. PMID: 15770055.
Prevete N et al. Helicobacter pylori HP(2-20) induces eosinophil activation and accumulation in superficial gastric mucosa and stimulates VEGF-alpha and TGF-beta release by interacting with formyl-peptide receptors. Int J Immunopathol Pharmacol. 2013 Jul-Sep;26(3):647-62. doi: 10.1177/039463201302600308. PMID: 24067461.
Band cell. Wikipedia. https://en.wikipedia.org/wiki/Band_cell. Accessed 10 November 2022.
By Bobjgalindo. English: Band neutrophil from a blood smear under a microscope (40x). Español: Neutrófilo en cayado o en banda de un frotis de sangre periférica (40x). Own work. 12 March 2005. Creative Commons Attribution-Share Alike 4.0 International 3.0 Unported, 2.5 Generic, 2.0 Generic and 1.0 Generic license.
By Yikrazuul. English: structure of Homo sapiens DNA polymerase beta, pdb file 7ICG. A bound DNA is also indicated. 25 July 2009. Creative Commons Attribution-Share Alike 3.0 Unported license.
DNA polymerase. Wikipedia. https://en.wikipedia.org/wiki/DNA_polymerase. Accessed 18 November 2022.
Calam J et al. How does Helicobacter pylori cause mucosal damage? Its effect on acid and gastrin physiology. Gastroenterology. 1997 Dec;113(6 Suppl):S43-9; discussion S50. doi: 10.1016/s0016-5085(97)80010-8. PMID: 9394759.
Aline Cristina Targa Cadamuro et al. Helicobacter pylori infection: Host immune response, implications on gene expression and microRNAs. World J Gastroenterol. 2014 Feb 14; 20(6): 1424-1437. Published online 2014 Feb 14. doi: 10.3748/wjg.v20.i6.1424. PMCID: PM3925852. PMID: 24587619.
Leukocyte extravasation. Wikipedia. https://en.wikipedia.org/wiki/Leukocyte_extravasation. Accessed 20 January 2023.
By y _tambe. Diagram of gastric ulceration by H. pylori, with English annotation 1. H. pylori penetrate the mucus layer of host stomach and adhere the surface of gastric mucosal epithelial cells. 2. produce ammonia from urea by the urease, and the ammonia neutralize the gastric acid to escape from elimination. 3. prolifirate, migrate, and finally form the infectious focus. 4. The gastric ulcerization is developed by destruction of mucosa, inflammation and mucosal cell death. 6 January 2006. dual-license with GFDL and CC-by-SA.